Why Is a Second Blood Pressure Reading Lower
Abstract
Nosotros evaluated the consequences of excluding the first of three blood pressure (BP) readings in different settings: a random population sample (POS, n=1525), a full general practice office (GPO, north=942) and a specialized hypertension heart (SHC, n=462). Differences between systolic and diastolic BP (SBP and DBP) estimates obtained including and excluding the first reading were compared and their correlation with convalescent BP monitoring (ABPM) was estimated. The samples were divided into quartiles according to the departure between the third and the first SBP (three-1ΔSBP). SBP decreased through sequential readings, 3-1ΔSBP was −5.5±9.7 mm Hg (P<0.001), −5.1±x.4 mm Hg (P<0.001) and −6.i±ix.3 mm Hg (P<0.001) for POS, GPO and SHC, respectively. Still, individuals included in the top quartile of three-1ΔSBP showed their highest values on the 3rd reading. The mean SBP gauge was significantly college excluding the get-go reading (P<0.001), but the differences amidst both approaches were small (ane.v–1.6 mm Hg). Moreover, the correlation betwixt SBP values including and excluding the first reading and daytime ABPM were comparable (r=0.69 and 0.68, respectively). Similar results were observed for DBP. In conclusion, our report does not support the notion of discarding the kickoff BP measurement and suggests that it should exist measured repeatedly, regardless the first value.
Introduction
Accurate function blood pressure (BP) measurement remains the mainstay of the diagnosis and treatment of hypertension, and the BP estimate in the first visit is the cornerstone of the initial management of hypertension as these values will be used to decide if subsequent visits are necessary. The recognition of a reduction in the white-coat consequence through successive measurements of BP1 has led to the proposition that discarding the first office reading of a set of three may improve the possibility of knowing the actual BP. If BP always decreases in the subsequent measurements, additional BP readings are not necessary when the offset measurement is <140/ninety mm Hg. However, the assumption that the first BP reading is systematically college in all subjects was not widely studied. 2 guidelines aimed at improving hypertension diagnosis and treatment in the clinical exercise were recently published, the '2013 European Society of Hypertension (ESH) and of the European Gild of Cardiology (ESC) guidelines for the management of arterial hypertension'2 and the '2013 Canadian Hypertension Teaching Program (CHEP) Recommendations for Blood Pressure Measurement, Diagnosis, Cess of Risk, Prevention, and Handling of Hypertension'.3 They hold on a value of ⩾140/ninety mm Hg as hypertension threshold, but there is disagreement regarding whether the first reading should be discarded or not. The ESH/ESC guidelines recommend taking 'at least two BP measurements, in the sitting position, spaced 1–ii min autonomously, and additional measurements if the first two are quite different'. On the other hand, the Canadian guidelines suggested that 'At the initial visit for the assessment of hypertension, if systolic BP is ⩾140 and/or diastolic BP is ⩾90 mm Hg, more than ii additional readings should be taken during the same visit' and 'The first reading should be discarded and the latter two readings averaged'.
Disagreement about whether to discard the first BP measurement or non was as well observed in population studies; for example, ii recently published studies aimed at evaluating the variability of BP in the general population—both based on National Health and Nutrition Examination Survey (NHANES) information—estimated the BP using different criteria: the first used the boilerplate of the second and third measurement4 whereas the other used the average of the three readings.5
The aim of our study was to evaluate the upshot of discarding the first BP measurement. For this purpose the BP estimates including and excluding the offset reading were compared in 3 different settings: (a) a random population sample, (b) a screening for loftier BP in general exercise offices (GPOs) and (c) a specialized evaluation in a hypertension center. In the last setting we also evaluated whether discarding the first BP reading improves the human relationship between office BP and ambulatory BP monitoring (ABPM) as was previously suggested.
Materials and methods
The report was performed using information from individuals who had had at least iii consecutive BP readings on ane occasion from three independent samples, (1) a random population sample, (2) consecutive patients in a GPO and (iii) sequent patients in a specialized hypertension heart (SHC).
The methodology used in the random population sample to obtain measurements has already been published.half dozen,vii In brief, three BP measurements spaced around 2 min from one some other were performed at home by trained nurses, after a minimum resting flow of v min, using a mercury sphygmomanometer. Stage I and V Korotkoff sounds were used to place systolic BP (SBP) and diastolic BP (DBP) respectively.
In the GPOs, doctors using the OMRON HEM 705 CP devices (OMRON HEALTHCARE Co., Kyoto, Japan) took iii BP measurements separated by a minute in a single visit from every patient examined regardless of the purpose of the visit.
In the SHC especially trained nurses performed three BP measurements just before the realization of ABPM with the same device and methodology used in the GPO setting. The ABPM registries were performed with the SpaceLabs 90207 monitor (Spacelabs Healthcare, Issaquah, WA, Usa) programmed to read BP at intervals of 20 min during the twenty-four hours and xxx min during the night. Day and dark was differentiated past taking into account the patient'due south diary.
To clarify the BP behavior through successive readings and evaluate if the outset reading was systematically highest, hateful and quartiles of the difference betwixt the third and first SBP (3-1ΔSBP) and DBP (3-1ΔDBP) readings were estimated. In social club to make up one's mind the effects of antihypertensive drugs, individuals with and without treatment were analyzed separately. Historic period and body mass index were compared amongst quartiles of 3-1ΔSBP using analysis of variance with Tukey postal service hoc analysis, and sex activity and current smoking using χ 2-test.
To estimate the effect of discarding the offset BP reading, mean BP was estimated in each subject area using two unlike approaches: (ane) discarding the commencement measurement and (ii) averaging the three readings.
Differences between SBP and DBP values obtained using both approaches were calculated and compared using i-sample t-test. Also, for each sample, Bland–Altman plots were synthetic with the difference of the two approaches on the vertical centrality and the average of the two approaches on the horizontal axis. Horizontal reference lines on the scatterplot showed the departure between the measurements ±2s.d. In order to investigate the cyclopedia of high BP diagnosis (SBP⩾140 mm Hg and/or DBP⩾90 mm Hg) among both BP estimates, nosotros calculated the kappa coefficient (κ) afterward dichotomizing the function measurements as 'loftier' or 'low' BP. The prevalence of high BP both including and excluding the starting time BP reading were compared using McNemar'southward exam.
Finally, in the SHC sample, the relationship between the office BP values obtained and the mean daytime ABPM were evaluated using Pearson correlation coefficient (r); additionally, 95% confidence intervals (95%CI) for r values were calculated based on the Fisher r-to-z transformation.
Statistical analyses were performed using SPSS 18.0 software (SPSS, Chicago, IL, USA); ii-tailed P-values <0.05 were considered statistically significant.
Results
The written report included 2926 individuals (1780 women, 46±17 years erstwhile and 1149 men, 47±17 years old, P between sex activity=0.566). The characteristics of the iii samples are described in Table 1.
As Tables 2 and three show, mean BP decreased across the sequential readings; the mean decrease was similar in all settings; Δ3-1SBP was −5.5±ix.seven mm Hg (P<0.001), −5.1±10.4 mm Hg (P<0.001) and −vi.1±9.3 mm Hg (P<0.001) in the random population sample, GPO and SHC, respectively; Δ3-1DBP was −3.0±9.0 mm Hg (P<0.001), −1.71±7.eight mm Hg (P<0.001), and −ii.1±5.7 mm Hg (P<0.001) in the random population sample, GPO and SHC, respectively. However, when the samples were divided into quartiles of the Δ3-1SBP, the individuals included in the superlative quartile had higher SBP values in the third reading compared with the outset i (Effigy 1a); like beliefs was observed with DBP when it was divided into quartiles of Δ3-1DBP (Figure 1b). Individuals in the pinnacle quartile of Δ3-1SBP were younger (46±18 vs 49±xvi years old, P=0.007) and thinner than individuals in the first quartile of (trunk mass index 26.7±5.4 vs 28.ane±6.6, P<0.001). The percentage of current smokers was higher in the height quartile of Δ3-1DBP than in the remaining quartiles (26.4 vs 22.vi, P=0.034). The percentage of women was similar amidst quartiles of Δ3-1SBP (61.2, 62.five, 61.6 and 58.0, P=0.284).
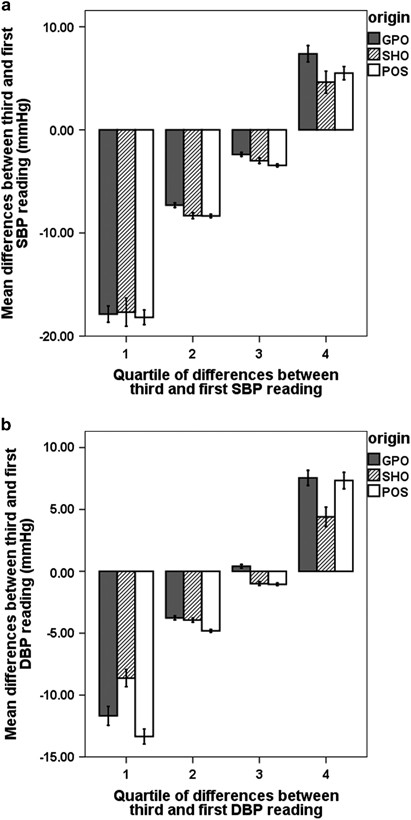
Hateful differences betwixt the third and the start SBP (a) and DBP (b) readings according to quartiles of these differences in the iii samples analyzed: random population sample (POS), general exercise office (GPO) and specialized hypertension office (SHO).
Tables 2 and 3 likewise compare the departure betwixt the mean of all readings and the mean excluding the beginning reading; SBP and DBP were significantly lower in all settings when the first reading was discarded. Although the hateful differences for SBP including and excluding the showtime BP reading seem only small, ane.5 (three.0), 1.6 (ii.8) and 1.6 (ii.8) mm Hg for GPO, specialized hypertension and role random population sample, respectively (Table 2), the range was wide, and included positive and negative values (from −xiii.3 to 27.iii mm Hg) (Effigy 2, Bland–Altman plots). Therefore, excluding the first reading did not yield lower values systematically. Similar results were obtained for DBP (Table iii); the mean differences between BP estimates were 0.5 (ii.3), 0.6 (1.seven) and 0.8 (two.half-dozen) mm Hg for GPO, specialized hypertension and office random population sample, respectively.
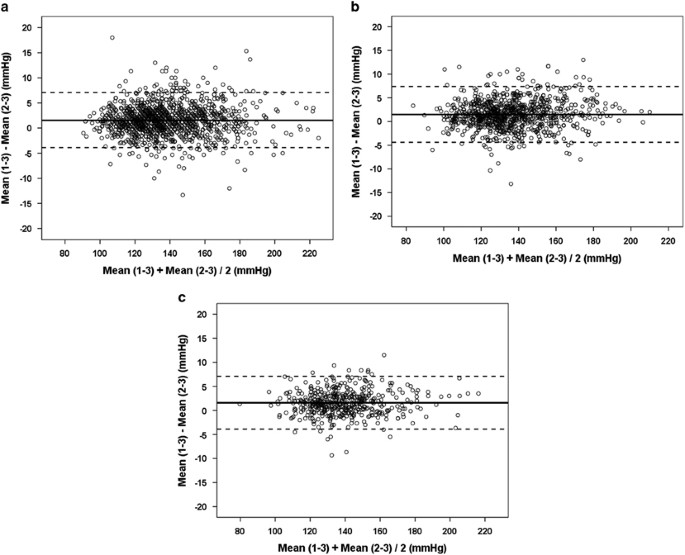
Bland–Altman plots comparing the SBP approximate using the mean of three readings and discarding the first reading in the three samples analyzed: random population sample (POS) (a), full general exercise office (GPO) (b) and specialized hypertension office (SHO) (c).
The proportion of individuals with 'high' BP (⩾140/xc mm Hg) was lower when the get-go reading was excluded in all settings (42.3% vs 44.half dozen% in the random population sample, P<0.001, 42.three% vs 44.three% in the GPO, P=0.005 and 45.v% vs 48.vii% in the SHC, P=0.001). However, the concordance betwixt approaches was loftier (κ=0.90, 0.91 and 0.91 for the random population sample, the GPO and the SHC, respectively); indeed, 2794 of 2929 subjects were classified concordantly; amid the 135 subjects classified discordantly, 75.six% were considered as 'high' BP but when the mean of all three readings was used and 24.four% when the first BP reading was excluded.
In the SHC sample, 446 ABPMs were considered valid. The correlations betwixt daytime systolic ABPM and both approaches to judge function SBP were small but similar, r=0.69 (95% CI 0.64–0.73, P<0.001) and r=0.68 (95% CI 0.61–0.73, P<0.001), for the mean of three readings and excluding the first measurement, respectively (Figure three). The correlations between daytime diastolic ABPM and office DBP estimates were also similar, r=0.69 (95% CI 0.64–0.73, P<0.001) and r=0.68 (95% CI 0.63–0.73, P<0.001), respectively.
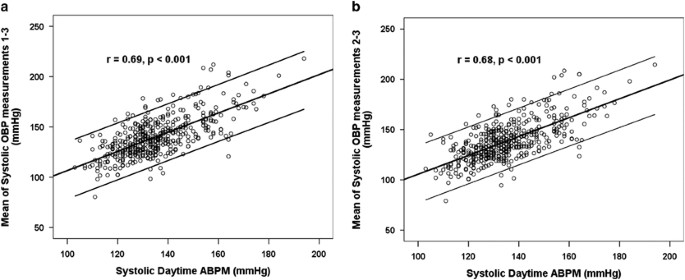
Pearson's correlation betwixt systolic daytime ambulatory blood pressure level monitoring (ABPM) and the role systolic blood pressure (OBP) estimate obtained using (a) the mean of three readings and (b) discarding the first reading.
Word
Accurate part BP measurement, despite its shortcomings, remains the mainstay of diagnosis and treatment of hypertension. Withal, the simple question of whether the first office BP measurement should exist discarded remains to be answered and at that place is no understanding among the varying hypertension guidelines. Thus, the Canadian3 and Prissy8 guidelines recommend discarding the first BP measurement, whereas the ESH/ESC one does not.ii Our information evidence that, in all settings analyzed, the effect of excluding the first BP reading was significant just small, ~1.5 and <1 mm Hg for SBP and DBP, respectively. Moreover, when BP was analyzed as a dichotomic variable in gild to classify subjects every bit 'high' or 'depression' BP, the vast bulk were classified concordantly.
Information technology has been suggested that excluding the first BP measurement could improve the correlation between part BP and out of the office BP. However, our data do not back up this concept; using the second and third readings only (that is, discarding the first) did non improve the correlation with daytime ABPM when compared with the utilize of hateful of all three readings; indeed, r values were almost identical whether the first BP measurement was included or not. This statement is concordant with a previously published study about untreated hypertensive patients9 merely expands the conclusion to non-hypertensive subjects and to subjects using antihypertensive drugs.
The decrease of BP in successive measurements has been shown repeatedly and with different methods,ten and information technology is widely internalized in medical thinking that successive measurements will requite lower BP values. Thus, Parati et al. 4 suggested that discarding the starting time reading may improve the accuracy of the diagnosis of hypertension. Furthermore, in order to eliminate the increment of BP associated with the effect of alarm, ESH guidelines for dwelling house BP measurement recommend discarding the measurements performed on the offset day.11 Still, the scientific testify to back up these assumptions is minimal and valuable data near BP variability could be lost.
Possibly the virtually interesting finding in our report was the fact that ~25% of the individuals did not decrease or increment their BP trough successive measurements and, consequently, in these individuals the first reading was non the highest. Remarkably, this behavior was found in all three settings (population sample, general practice and specialized hypertension function) and it was as well contained of whether BP was measured by medical doctors or nurses, in the office or at home. Despite this phenomenon being previously published,12 information technology is not widely recognized and it has several implications for clinical do.
Commencement, the consequences of excluding the initial reading are unpredictable for an individual patient. As Bland–Altman plots prove, the differences among BP estimate excluding or including the beginning measurement were wide, and yield both positive and negative values. Indeed, although the individuals who increased their BP in the third reading were younger, thinner and more current smokers than those who decreased BP trough successive measurements (start quartile of 3-1ΔSBP), there are no practical means to identify them. Interestingly, the reclassification of individuals in categories of BP using the mean of the first and second, first through tertiary, and second and tertiary readings was recently published.13
Another related issue is whether or not a dr. should take more readings simply when the first is ⩾140/ninety mm Hg as the NICE guidelines and Canadian recommendations suggest; our findings practice non support this approach. Every bit the cardiovascular chance has a continuous relationship with BP starting with values equally depression as 115/75 mm Hg,14 taking only one BP measurement could significantly underestimate the discipline's 'true' hazard of cardiovascular consequence.
Finally, the divergence betwixt the first and third reading could give some important information about the BP variability. There is now some evidence that several such representations of BP variability, if augmented, increase cardiovascular risk independent of the boilerplate of BP readings conventionally acquired.15 Visit-to-visit SBP variation was linked to increased cardiovascular and stroke mortality risk.xvi Although the risk associated with the short-term variability has been studied less, the BP variation in one visit results from changes in heart rate, stroke volume and peripheral resistance in response to external and internal stimuli and their importance in terms of the risk of developing hypertension or cardiovascular disease remain to be defined.
Some limitations of our study have to exist pointed out. Starting time, this was a post hoc analysis. 2nd, this study was performed in unlike settings with different methodologies to measure BP. However, our findings were concordant through all the samples, suggesting that the BP patterns observed were strongly consistent. Finally, our study was not able to define whether one approach would exist more appropriate than some other; only long-term prospective studies with hard stop points could provide a definitive answer.
In conclusion, our study does not support discarding the offset BP measurement every bit the Canadian and Dainty guidelines have suggested. Remarkably, although the mean BP decreased in successive BP readings, the behavior of individuals was unpredictable and an appreciable proportion of subjects had the highest BP value in the concluding reading. We suggest that three BP readings should be taken in all individuals independently of the first reading value.
References
-
Parati G, Mancia G . Assessing the white coat effect: which claret pressure measurement should be considered? J Hypertens 2006; 24: 29–31.
-
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm G et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the task force for the direction of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
-
Hackam DG, Quinn RR, Ravani P, Rabi DM, Dasgupta Grand, Daskalopoulou SS et al. The 2013 Canadian Hypertension Teaching Programme recommendations for claret pressure level measurement, diagnosis, assessment of adventure, prevention and handling of hypertension. Tin can J Cardiol 2013; 29: 528–542.
-
Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S . The human relationship betwixt visit-to-visit variability in systolic blood force per unit area and all-crusade mortality in the general population: findings from NHANES 3, 1988–1994. Hypertension 2011; 57: 160–166.
-
Muntner P, Levitan EB, Reynolds Chiliad, Mann DM, Tonelli M, Oparil S et al. Inside-visit variability of claret pressure and all-cause and cardiovascular mortality among US adults. J Clin Hypertens (Greenwich) 2012; fourteen: 165–171.
-
Salazar MR, Carbajal HA, Aizpurúa Thousand, Riondet B, Rodrigo HF, Rechifort V et al. Decrease of claret force per unit area by community-based strategies. Medicina (B Aires) 2005; 65: 507–512.
-
Salazar MR, Carbajal HA, Espeche WG, Aizpurúa M, Leiva Sisnieguez CE, March CE et al. Identifying cardiovascular illness hazard and outcome: utilise of the plasma triglyceride/high-density lipoprotein cholesterol concentration ratio versus metabolic syndrome criteria. J Intern Med 2013; 273: 595–601.
-
National Clinical Guideline Center (Britain). Hypertension: The Clinical Management of Master Hypertension in Adults: Update of Clinical Guidelines xviii and 34 [Internet]. Royal College of Physicians (Britain): London, 2011.
-
Graves JW, Grossardt BR . Discarding the kickoff of three nurse-auscultatory or oscillometric claret pressure level measurements does not improve the association of office claret pressure with ABPM. Blood Press Monit 2010; 15: 146–151.
-
Mengden T, Hernandez Medina RM, Beltran B, Alvarez Eastward, Kraft One thousand, Vetter H . Reliability of reporting cocky-measured blood pressure values past hypertensive patients. Am J Hypertens 1998; 11: 1413–1417.
-
Parati One thousand, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y et al. ESH Working Grouping on Blood Pressure Monitoring European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens 2010; 24: 779–785.
-
Graves JW, Grossardt BR, Gullerud RE, Bailey KR, Feldstein J . The trained observer better predicts daytime ABPM diastolic blood pressure in hypertensive patients than does automatic (Omron) device. Blood Press Monit 2006; 11: 53–58.
-
Handler J, Zhao Y, Egan BM . Touch of the number of blood pressure level measurements on blood pressure level classification in Us adults: NHANES 1999–2008. J Clin Hypertens (Greenwich) 2012; 14: 751–759.
-
Lewington S, Clarke R, Qizilbash North, Peto R, Collins R . Prospective Studies Collaboration. Age-specific relevance of usual blood force per unit area to vascular mortality: a meta-assay of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913.
-
Floras JS . Claret pressure variability: a novel and important take chances gene. Can J Cardiol 2013; 29: 557–563.
-
Kikuya Yard, Ohkubo T, Metoki H, Asayama K, Hara A, Obara T et al. Solar day-past-day variability of claret force per unit area and middle charge per unit at home as a novel predictor of prognosis: the Ohasama Study. Hypertension 2008; 52: 1045–1050.
Acknowledgements
This study could not take been conducted without the help of the nurses from the 'Hospital Municipal, San Andrés de Giles' and the 'Hospital Municipal, Rauch' and the nurse Miriam Susana Cor from the 'Infirmary Universitario San Martín, La Plata'. Nosotros appreciate the assist of Sonja Zander in the revision of the English language of this manuscript.
Author information
Affiliations
Respective author
Ideals declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Salazar, M., Espeche, W., Aizpurúa, G. et al. Should the first blood pressure reading be discarded?. J Hum Hypertens 29, 373–378 (2015). https://doi.org/10.1038/jhh.2014.98
-
Received:
-
Revised:
-
Accepted:
-
Published:
-
Issue Date:
-
DOI : https://doi.org/10.1038/jhh.2014.98
Source: https://www.nature.com/articles/jhh201498
Post a Comment for "Why Is a Second Blood Pressure Reading Lower"